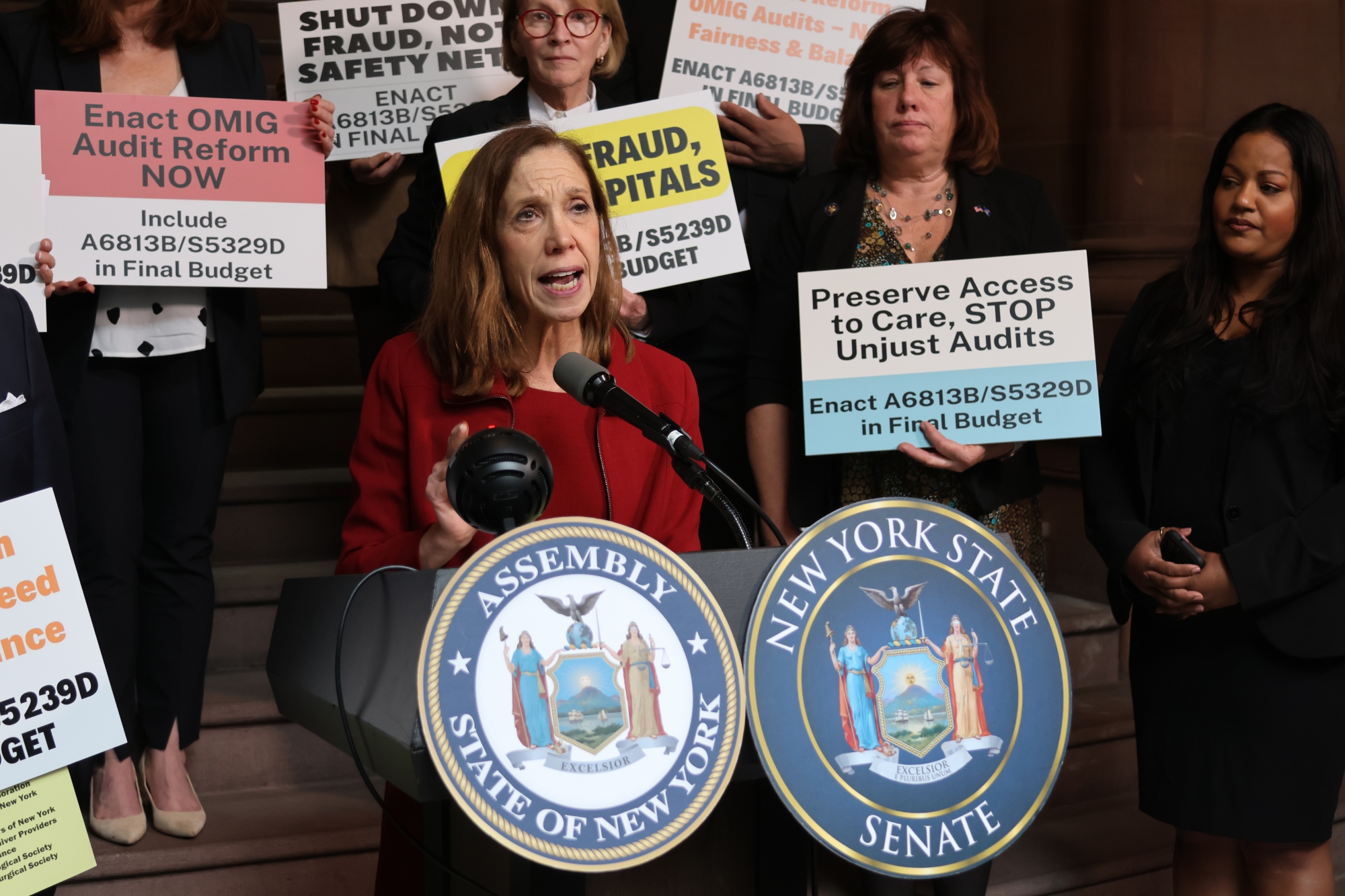
Assemblywoman Amy Paulin, State Senator Pete Harckham and Providers Unite to End Unfair, Punitive Medicaid Auditing Practices
Healthcare providers are being punished and financially crippled for clerical errors
Albany, NY – Assemblywoman Amy Paulin (D-Scarsdale), State Senator Pete Harckham (D-Lewisboro) legislators and advocates spoke in unison at the Capitol today, calling for the state budget to include meaningful reform of current practices utilized by the NYS Office of the Medicaid Inspector General (OMIG) when it audits healthcare agencies that provide essential services to New Yorkers with Medicaid insurance.
Providers who operate in good faith and deliver high quality care live in fear of OMIG audits because they can be punished severely for technical errors that are not material to whether the Medicaid recipient received the service, or the quality of care provided.
Current OMIG audit practices include application of extrapolation to clerical errors, which has resulted in disproportionate findings and enormous fines that can shut down an entire program or impacted Medicaid provider. This practice has been devastating to providers and risks the continued viability of New York’s safety net system.
A new OMIG reform bill A.6813-B (Paulin)/S.5329-D (Harckham) seeks to rectify tactics used during Medicaid audits conducted by the OMIG that are needlessly punitive and, ultimately, ineffective in preventing fraud and abuse in the healthcare system. These audits take time and resources away from healthcare and mental hygiene agencies providing essential services to New Yorkers with Medicaid insurance.
Paulin and Harckham’s legislation addresses concerns regarding the need to ensure the state’s continued ability to address fraud and abuse and meeting all federal requirements and auditing expectations of the State, while also assuring that an already stretched and understaffed Medicaid provider community is not inappropriately burdened or unfairly punished.
Assemblywoman Amy Paulin said, “The role of the NYS Office of the Medicaid Inspector General is to root out fraud and abuse. However, this should not mean that OMIG should have the ability to wipe out entire programs and services based on technical errors, state system issues, or minor discrepancies, especially when the service was delivered appropriately. This practice is crippling and risks the continued viability of New York’s safety net system. I urge the Legislature to include the provisions of S.5329-B/A.6813-A in the budget to protect our health care providers and safeguard OMIG’s role in assuring Medicaid’s integrity.”
Senator Pete Harckham said, “New York patients cannot afford to lose any more behavioral health providers, especially over unintentional administrative errors. The senseless undermining of Substance Use Disorder programs in the middle of an opioid epidemic needs to stop. Let’s not lose sight that these programs save lives, so regulatory efforts should be in line with supporting and improving services, not harming them.”
OMIG reform also has broad support from representatives and healthcare providers across the state:
Assemblymember John T. McDonald III, RPh, who has the unique perspective on Medicaid audits as a legislator and registered pharmacist, said, "Within our Medicaid auditing system, it is essential to recognize the delicate balance between oversight and support for our healthcare providers. The Legislature's inclusion of reform legislation in the budget signifies a crucial step towards rectifying current issues within OMIG auditing practices. It reflects a commitment to safeguarding both the integrity of the Medicaid program and the sustainability of our healthcare providers. While setbacks were faced in the past, the introduction of bill S.5329-D (Harckham)/A.6813-B (Paulin) underscores our collective determination to find a solution that upholds accountability without unduly punishing those on the frontlines of care.
Now is the time to enact meaningful reform that strikes the necessary balance. By doing so, we can ensure that our Medicaid program remains robust, fair, and responsive to the needs of all New Yorkers."
"For over 10 years the New York State Council and our colleagues from across New York's healthcare continuum of care have been fighting for OMIG audit reforms that will infuse balance, fairness and greater transparency in all areas of the OMIG audit process,” said Lauri Cole, Executive Director, New York State Council for Community Behavioral Healthcare. “We are grateful to Senator Harckham and Assemblywoman Paulin for sponsoring our current 'same as' legislation (S5329D/A6813B) and to both houses of the legislature for acknowledging the need for audit reform.Our bill addresses the concerns that have been raised regarding previous versions of the legislation and as such we are 100% confident the language is consistent with OMIG's mission and will not in any way tie the hands of the Office as it preforms its core functions. Some of the tactics used by OMIG go far beyond its core mission and threaten access to care for thousands of Medicaid members who rely on Medicaid safety net providers across the state.The time is now for meaningful reform."
“Currently, the tactics used during Medicaid audits conducted by the NYS OMIG are needlessly punitive and, ultimately, ineffective in preventing fraud and abuse in the healthcare system,” said Assembly Member Harvey Epstein. “Recently, ParkMed, a highly respected and essential abortion provider in my district, was targeted during this process and has been fined nearly $1 million for correctable technical errors due to switching to a new electronic billing system. We need a more fair, reasonable OMIG auditing process and that is why I support the passage of S.5329-D (Harckham)/A.6813-B (Paulin) this session”.
Winifred Schiff, CEO of Inter Agency Council of Developmental Disabilities Agencies, Inc, said, “Extrapolation on clerical errors does not eliminate fraud, abuse or waste.Instead, it threatens the existence of already scarce services at a time when the need for them is overwhelming and growing.We need to correct this fundamentally misguided policy, now!”
Allegra Schorr, President of The Coalition of Medication-Assisted Treatment Providers and Advocates of New York State (COMPA), stated: "New York lost 6,900 lives to overdose last year and our rates from overdose deaths driven by fentanyl continue to rise. Opioid Treatment Programs (OTPs) and Medication-Assisted Treatment providers are on the frontlines.New York's Opioid Treatment Programs provide lifesaving treatment to more than 43,000 New Yorkers who are battling opioid addiction and the overdose epidemic.But our ability to do this vital work is in jeopardy, and we strongly urge the passage of S.5329-D/A.6813-B that calls for a much-needed reevaluation of OMIG’s audit process and statutory protections that prevent OMIG’s actions from leading to a reduction in access and services when no fraud or abuse is found.”
“No provider should be unfairly punished for making an honest mistake or error in their efforts to be paid for services rendered as a provider of Medicaid services, and this bill will help ensure administrative errors do not carry the same penalties as are warranted by actual fraud.The Medicaid provider network is already strained to the point of near failure in many parts of the State, and we’re happy to see the legislature is injecting a dose of common sense to the Medicaid audit process,” said Mike Alvaro, President and CEO of CP State.
Rose Duhan, Community Health Care Association of NYS President and CEO said, “CHCANYS appreciates the importance of eradicating fraud, waste, and abuse within New York’s Medicaid program. But OMIG’s current one-size-fits-all audit approach ends up severely penalizing already cash-strapped and understaffed providers for honest mistakes – forcing them to spend exorbitant amounts of time and money that would otherwise be spent treating patients and expanding access to care in underserved communities. CHCANYS urges NYS to include S5329D (Harckham)/A6813B (Paulin) in the State Budget to ensure that OMIG can do its work while creating protections and procedures that allow Medicaid service providers like Community Health Centers to continue delivering high-quality care to the patients who need it most.”
“New York’s behavioral health sector serves the most vulnerable among us, yet it struggles to maintain its workforce due to chronic underfunding of the system. OMIG’s draconian audit practices threaten the stability of this sector when demand for mental health and substance use services are only increasing.S.5329D/A6813B would provide a fair and reasonable approach to the Medicaid audit process that would not bankrupt already struggling providers who are offering legitimate, life-saving services,” said Assembly member Aileen Gunther, chair of the Assembly Committee on Mental Health.
"The New York State Psychiatric Association (NYSPA) supports S.5329-D/A.6813-B as it strikes a necessary balance between the need to protect OMIG’s mandate to eliminate fraud, waste and abuse in the Medicaid system and the need to ensure fairness and reasonableness for providers during the audit investigation process," said Rachel Fernbach, Executive Director and General Counsel.
"While OMIG audits are essential for weeding out fraud and abuse in New York's Medicaid system, current OMIG audit practices have become excessively punitive and many behavioral health service providers have paid a steep price for clerical errors made in good faith," said Senator Nathalia Fernandez. "These sensible reforms would bring fairness and transparency to the OMIG audit process, ensuring service providers are able to deliver high-quality care while allowing OMIG to continue performing its essential functions."
“The OMIG serves a critical role in combating fraud and abuse in the service system. We share the OMIG’s goals, both in our mission to deliver high-quality services and supports and our commitment to being fiscally responsible with the Medicaid funding that makes those services possible,” said Erik Geizer, CEO of The Arc New York. “These commonsense reforms will uphold the OMIG’s authority, but reduce the unnecessary burden on providers, which currently impede our partnership with OMIG and our ability to focus on quality care.”